
Doctors in the UK have genetically modified immune cells borrowed from healthy people to create a ‘living drug’ that stays in the body, fights and sometimes even reverses aggressive or ‘stubborn’ cancers in patients who don’t respond to other therapies.
The science is not entirely new. Doctors have in the past taken patients’ own immune cells (known as CAR-T), reprogrammed them with viruses to target cancer, and put them back into the body. “It was effective in patients with stubborn blood cancers. But this may take weeks to make, and can fail if patients are sick,” says paediatric haematologist Dr Revathi Raj.
Under the new therapy, donor cells (called base-edited CAR7-T) are drawn from healthy people. “The cells don’t have a virus risk, and are better trained to fight tricky T-cell (immune cells) cancers. They have built-in safety switches against rejection,” says Dr Raj. “The innovation is exciting because it’s faster, cheaper in the long run, and safer in patients with leukaemia.”
What cancers get treated?
For the 2025 study, published in the New England Journal of Medicine, scientists used donor cells to treat acute lymphoblastic leukaemia, a fast-progressing blood cancer originating in the bone marrow. In this condition, immature lymphocytes (lymphoblasts) multiply uncontrollably, crowding out healthy blood cells and weakening immunity, clotting and oxygen delivery.
It strikes about 65,000 people annually across the globe and comprises about a third of childhood leukaemias. In most paediatric cases, cancers aren’t preventable but are highly treatable, says senior paediatric oncologist Dr Julius Scott, director of the department of paediatric haematology-oncology at Dr Rela Institute and Medical Centre. “The survival rate of acute lymphoblastic leukaemia is more than 90% in children, but drops to 50% in adults. Unlike with adults, childhood cancers are not related to obesity and diabetes or environmental factors such as pollution.”
How does it work?
The donor cells are heavily edited using a precise form of gene editing — base editing — to make them ‘universal’ so they can be used in different patients without needing a perfect tissue match. Donor white blood cells, or T cells, are modified to hunt down cancer cells in patients with acute lymphoblastic leukaemia.
The future?
The study shows that BE-CAR7 T cells can safely and effectively bring stubborn T-cell leukaemia into remission, making stem-cell transplantation possible for most patients. Doctors, however, warn of long-term risks such as infection after transplant or relapse. The US FDA requires companies that make CAR-T cells for therapy to add a boxed warning that the treatments may cause cancer. While noting that risks outweigh benefits, the agency has said patients must be monitored for secondary cancers.
-
Hindu Man Lynched: Bangladesh To Take Responsibility Of Victim's Family

-
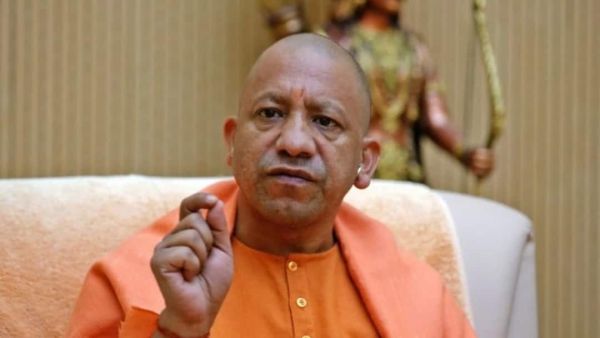
UP Codeine Syrup Row: Rs 50,000 Reward On Key Accused, Yogi Govt Signals Zero Tolerance
-
'Hindus Must Be Safe': Janhvi Kapoor's Boyfriend Shikhar Pahariya Condemns Dipu Chandra Das' Brutal Lynching In Bangladesh

-
Star India cricketer reflects on Ishan Kishan’s return to T20 World Cup squad, says, ‘He gave…’

-
New Zealand name T20I and ODI squads for India tour, Michael Bracewell to captain ODIs, Kane Williamson…
