Joint pain affects millions worldwide and remains one of the most common causes of disability. Most people will experience knee or hip pain at some point. These weight-bearing joints endure constant strain while still allowing mobility. Wear and tear, injuries, or genetic factors often trigger the discomfort.
Whether due to osteoarthritis, tendinopathies, or age-related degeneration, the typical response hasn't changed much: painkillers, ice or heat packs, physiotherapy, and eventually, surgery if symptoms worsen. But these are often temporary fixes, not long-term solutions.
But as the science of healing evolves, so does the ambition of treatment. Orthopaedic and regenerative medicine specialist Dr Sharmila Tulpule believes that we are in the midst of a meaningful shift: from controlling symptoms to actually repairing the injured joint. "In the past decade or so, regenerative medicine has become a hopeful new area of orthopaedic medicine, moving the therapeutic emphasis from merely controlling pain to actually restoring and repairing injured tissue," she explains.
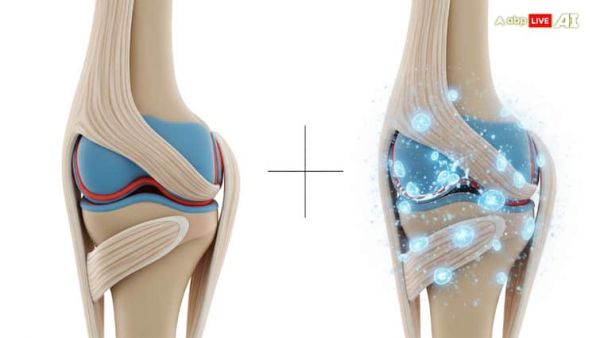
This approach taps into the body's natural capacity to heal itself, using refined elements from the patient's own blood, fat tissue, or cellular proteins. Such therapies are particularly promising for those in the early to moderate stages of joint disease, when some degree of natural tissue regeneration is still possible.
From Symptom Relief To Tissue Repair
The main differentiator in regenerative medicine is intent; traditional treatments often reduce pain temporarily, but rarely address the underlying degeneration. Dr. Tulpule points out that regenerative therapies instead aim to "stimulate cell proliferation, promote matrix repair, and modulate inflammation."
Take platelet-rich plasma (PRP), for instance. By spinning the patient's blood in a centrifuge, clinicians extract a high concentration of platelets, which are tiny blood components that release healing growth factors. These are then injected into the affected joint or tendon.
"It has been especially helpful in treating early-stage osteoarthritis, as it can reduce degeneration and enhance function and pain," Dr Tulpule notes.
Studies comparing PRP with traditional treatments like steroid or hyaluronic acid injections have found that PRP can offer better and longer-lasting results without the side effects of steroids. Since the material comes from the patient's own blood, the risk of rejection or allergy is minimal
Gold, Fat Cells And The Future Of Recovery
Another novel therapy on the horizon uses processed serum proteins activated by incubation with gold particles to encourage anti-inflammatory and healing responses in joints.
While gold might sound like something out of an alternative wellness brochure, the therapy's principle is solidly biological: the gold particles act as a stimulus for immune-modulating proteins, which are then reintroduced into the body in purified form.
"In diseases like osteoarthritis and chronic tendinopathies, this treatment aids in tissue repair, pain relief, and inflammation reduction," says Dr. Tulpule. "In contrast to steroids, regenerative healing promotes natural healing without suppressing the immune system."
Another approach gaining traction involves extracting regenerative cells from the patient's own fat tissue — a process that also yields a rich blend of stem cells and growth factors. These are carefully processed and reinjected into affected joints.
"Patients with multiple joint involvement and those with early to moderate osteoarthritis benefit most from adipose-derived therapy," she adds.
Again, the therapy is autologous—using the patient's own tissue—and minimally invasive, which makes it a safer option for those trying to avoid surgery.
A New Philosophy in Joint Care
While these treatments are not yet the default option in mainstream orthopaedics, their growing popularity — and research backing — suggests a changing tide. Still, Dr. Tulpule emphasises the importance of timely diagnosis and customised treatment planning.
"Regenerative medicine is revolutionising the way that joint pain is treated by utilising the body's natural ability to repair and regenerate rather than just covering up symptoms," she says. "Therapies like PRP…adipose-derived cells…provide a safer, more intelligent, and more sustainable route to recovery with proper diagnosis, early intervention, and a customised strategy."
For patients, this could mean more than just pain relief. It could mean the possibility of holding off surgery—or even avoiding it altogether—with the right therapy at the right time.
As the field continues to evolve, regenerative medicine is quietly rewriting the story of joint pain. Instead of a slow, inevitable decline, the future might just offer renewal.
Kirti Pandey is a senior independent writer.
-
ENG vs IND 2025: Irfan Pathan's old 2019 tweet resurfaces after Shubman Gill hits maiden double ton in Birmingham

-
ENG vs IND 2025: Irfan Pathan's old 2019 tweet resurfaces after Shubman Gill hits maiden double ton in Birmingham

-
How will Trump's 'Big Beautiful Bill' impact Americans?

-
How will Trump's 'Big Beautiful Bill' impact Americans?

-
M25 Dartford traffic LIVE: A282 now open to traffic after fuel spill caused 50 min delays
