Scientists at the University of Auckland in New Zealand have identified a specific brain region that may play a critical role in controlling blood pressure. This discovery challenges long-held beliefs and opens the door to new approaches in managing hypertension.
According to the study, a small area in the brainstem known as the lateral parafacial region (pFL) could be a key driver of high blood pressure. The brainstem connects the brain to the spinal cord and controls automatic body functions such as breathing, heartbeat, and digestion. Researchers have now found that this region is also linked to nerves that tighten blood vessels, which directly raises blood pressure.
In laboratory experiments conducted on rats with induced hypertension, scientists observed that the pFL region became unusually active. When this region was switched off, blood pressure levels dropped back to normal. This suggests that overactivity in this part of the brain may be responsible for maintaining high blood pressure in the body.
This discovery explains why some people develop hypertension even when they follow a low-salt diet, manage stress well, and maintain a healthy body weight. It also sheds light on why blood pressure sometimes remains high despite medication and lifestyle changes.
Experts say this does not mean salt and stress no longer matter. Instead, it shows that high blood pressure is far more complex than previously believed. The brain, nervous system, hormones, kidneys, and lifestyle factors all interact to regulate blood pressure.
Several other contributors still play a major role:
Lack of physical activity can cause blood vessels to stiffen over time, making it harder for blood to flow smoothly. Even thin people are at risk if they lead a sedentary lifestyle.
Kidney problems are strongly linked to blood pressure because the kidneys control fluid balance and sodium levels. When they do not function properly, pressure in the blood vessels rises.
Hormonal imbalances involving the thyroid or adrenal glands can also trigger abnormal blood pressure levels.
Poor sleep is another hidden factor. Sleeping less than six to eight hours regularly can disturb hormone regulation and activate stress responses that elevate blood pressure.
Excessive intake of tea, coffee, energy drinks, and smoking narrows blood vessels and stimulates the nervous system, causing sudden spikes in blood pressure.
Genetics also plays a powerful role. If high blood pressure runs in the family, a person may develop it regardless of weight, diet, or stress levels.
Dehydration, overuse of painkillers, and prolonged screen exposure can also contribute by affecting circulation, kidney health, and nervous system balance.
The discovery of the lateral parafacial region’s involvement means future treatments may focus on calming or regulating this part of the brain. This could lead to targeted therapies that go beyond conventional medicines that act only on the heart or blood vessels.
Researchers believe this finding may transform how doctors approach resistant hypertension — cases where blood pressure does not respond well to standard treatment. Instead of treating only symptoms, therapy could focus on correcting the brain’s signals that control blood vessel tension.
This research also reinforces the importance of a holistic approach to health. Managing blood pressure is not just about reducing salt or stress. It involves:
Regular physical activity
Balanced sleep cycles
hydration
Controlled caffeine intake
Avoiding tobacco
Protecting kidney and hormonal health
Managing screen time
Monitoring genetic risks
High blood pressure is often called a “silent killer” because it shows few early symptoms but damages the heart, brain, kidneys, and eyes over time. Understanding that the brain itself can initiate the problem helps explain why prevention must be broader and more integrated than before.
The brain’s lateral parafacial region may be small, but its influence on blood pressure appears powerful. This discovery marks a shift from viewing hypertension as only a lifestyle disease to recognizing it as a neurological and systemic condition.
Disclaimer: This article is for general awareness only. It does not replace medical advice. Individuals with high blood pressure should consult qualified healthcare professionals for diagnosis, treatment, and personalized care.
-
IND Vs NZ Final ODI: 'Chase Master' Virat Kohli Slams 78th Half-Century In Series Decider

-
Eternity OTT Release Date: When & Where To Watch Elizabeth Olsen's Latest Romantic Fantasy Film?

-
Virat Kohli’s HEROIC in vain as New Zealand clinch historic first ODI series win in India

-
Real reason King Charles 'will not see' Prince Harry next week

-
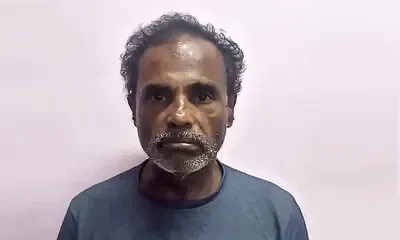
Notorious thief arrested in attempted theft case in Karkala